In honour of Biomedical Science day 2021, I reached out to the Biomedical Science Community to host interviews with Biomedical Scientist’s in different disciplines. My aim is to raise awareness of what Biomedical Scientist’s do in different disciplines.
My first interview is with Norman Fry Consultant Clinical Scientist and Laboratory Surveillance Lead for Vaccine Preventable Bacteria in the Immunisation and Countermeasures Division, Public Health England – National Infection Service, London.
Hi Norman, could you tell me about your roll as a scientist?
“Hi Muneebah, thanks for invitation. My name is Norman Fry @NormFry2013 and I am a Consultant Clinical Scientist and Laboratory Surveillance Lead for Vaccine Preventable Bacteria in the Immunisation and Countermeasures Division, Public Health England – National Infection Service, London @PHE_UK. I am responsible for the development of new initiatives and implementing new policies/maintaining existing policies. I actively engage with medical, epidemiological and laboratory colleagues. I am responsible for the delivery of results through my team, which is made up of ten core healthcare scientists including Biomedical Scientists, Clinical Scientists and bioinformaticians together with five additional staff on fixed-term positions, students on rotation or completing projects. Together with my team our role is to inform the surveillance of vaccine preventable diseases by providing laboratory reference services for Bordetella pertussis(which causes whooping cough), Streptococcus pneumoniaeand Haemophilus influenzae(which can cause invasive diseases such as bacteraemia and meningitis), and toxigenic corynebacteria (which can cause respiratory or cutaneous diphtheria). We are the National Reference Laboratory for each of these organisms and our laboratory is also the World Health Organisation Global Collaborating Centre (CC) for Diphtheria & Streptococcal infections and is a WHO CC for Haemophilus influenzaeand Streptococcus pneumoniae. We are actively involved in number of national and international research projects. I am also Co-Editor-in-Chief of the Journal of Medical Microbiology (with Prof. Kalai Mathee, Florida International University, USA), a Microbiology Society journal”
https://www.microbiologyresearch.org/content/journal/jmm
@MicrobioSoc #JMedMicro.
Whilst you were in school what was you favourite subject school and what is your hobby?
“At school it was biology, which is how I got into microbiology, as it was one of the options for ‘A’ level Biology. Hobby-wise I like walking/hiking, photography and music (playing flute and guitar).”
What Is your favourite movie?
“Tough to choose one. Of the more recent ones I’ve seen I’d have to go with My Octopus Teacher, but going back a few years I also loved Little Miss Sunshine.”

How did you begin your career in Biomedical Science and What inspired you to work in this field?
“After finishing a BSc (Hons) degree in Microbiology and Virology at Warwick University in 1984, I literally just applied for any jobs where my degree looked relevant. Thirty applications and one successful interview later, I started as ‘Junior B’ Medical Laboratory Scientific Officer (MLSO) at the Public Health Laboratory Service’s Central Public Health Laboratory, Colindale, London (later the MLSOs became known as Biomedical Scientists). My first job was in the Division of Hospital Infection typing Lancefield Group A streptococci. My original ambition was to become a Forensic Scientist (this was before the days of Crime Scene Investigation (CSI) Vegas). But, I became fascinated by microbiology by watching amoebae engulf paramecium down a microscope. I can’t help having been influenced by my father who was also a microbiologist (a Reader in Microbiology at Sheffield University). Although to his credit he was so keen not to unduly influence my career choice he remained strangely silent until I had decided. I also thought about Environmental Science but eventually settled on Microbiology. I had a number of positions at Colindale. After my first post I moved to the Division of Enteric Pathogens to work on verotoxigenic Escherichia coli, then to the Division of Microbiological Reagents and Quality Control where I did my PhD on Legionella. I then moved to the USA to do a post-doc in Environmental Microbiology. On my return to England, I re-joined Colindale on a European Legionella project, and then moved to work with Vaccine Preventable Bacteria.”
Currently, what department do you work for?
“Now I work in Public Health England’s Immunisation and Countermeasures Division.
Can you tell me a little bit about what a reference microbiology lab?
“A reference microbiology laboratory performs a number of functions including specialist reference testing, provision of reference material and scientific advice, collaboration and research, surveillance and response. The data from our reference laboratory testing combined with epidemiological data helps to inform any changes to national vaccine policy via presentation to the Joint Committee on Vaccination and Immunisation (JCVI).”
What is the difference between a reference microbiology lab and a hospital microbiology lab?
“I would say the main difference is that hospital labs are front-line offering primary diagnostic testing to patients, whilst the reference labs offer specialist testing for diagnostics and surveillance which is not usually available in the hospital labs. For example our laboratory is the only one in the UK to offer toxigenicity testing of corynebacteria.”
Did your lab play a role throughout the pandemic?
“Yes and it still is. Public Health England’s COVID-19 response has affected us all. Various rotas have been introduced and members of my team have been involved with setting up SARS-CoV-2 PCRs to test specimens from patients and from various surveys including schools and in the technical and clinical validation for reporting of results. More recently the response has also expanded to include performing genotyping PCRs to identify the current variants (in addition to sequencing) which we are also supporting. Many of us are also participating in the ‘ESCAPE study’, a longitudinal seroepidemiological COVID-19 survey of PHE and NHS employees, with repeated collection of blood and oral fluid samples.”
In your laboratory what is a common organisms you look/ test for?
“Currently we receive clinical isolates of Bordetella pertussis(and other Bordetella species) for serotyping and further characterisation, Streptococcus pneumoniaeand Haemophilus influenzae(from cases of invasive diseases) for serotyping. We introduced routine whole genome sequencing (WGS) of invasive pneumococcal isolates to determine the serotype in October 2017. For H. influenzaefrom cases of invasive disease we determine the serotype using both PCR and typing antisera. Haemophilus influenzaeserotype b (Hib) can cause severe life-threatening disease in healthy individuals. Thanks to vaccination, Hib is now rare but if found requires follow-up action for prevention of secondary cases. We test potentially toxigenic corynebacteria (Corynebacterium diphtheriae, C. ulceransand C. pseudotuberculosis) for the presence of the diphtheria toxin gene by PCR and expression using a modification of the Elek test. We look for evidence of recent infection from pertussis in patients’ sera (and oral fluid from notified cases aged from 2 to <17 years old) by determining the antibody titre of anti-pertussis toxin IgG. We also test for immunity to diphtheria and tetanus in patient’s sera.”
Can you describe what a typical day or week is like for you?
“I’m not sure there is such a thing as typical because we have to react to what comes in on the day, but these days my week might include: checking in with my team, both onsite and offsite (via Teams) to see if there are any issues with the reference work and check on progress of projects. Clinical validation and reporting of results on our Laboratory Information Management System and telephoning out any urgent ones. I also attend incident management team meetings, for example when we do confirm a toxigenic corynebacteria from a patient. Preparing, reading and commenting drafts of manuscripts and guidance documents. Meetings with epidemiological and clinical colleagues to update in the various areas we cover and planning presentations for lectures and conferences (which lately have all been online).”
What is your favourite thing about your career?
“I believe our work does make a real difference. I enjoy seeing my team develop and the interaction between laboratory, epidemiology and clinical colleagues. I find the added dimension of bioinformatics to our work very exciting. I also find the collaborative nature of science both nationally and internationally, and my involvement with the Microbiology Society very rewarding.”
What motivates you to work hard?
“I would say my motivation comes from wanting to deliver the best services I can for public health.”
What are the greatest challenges you faced during your career?
“I think this depends on what stage you are at, so looking back probably trying to finish my PhD before moving to the USA to start my postdoc. Returning to the UK to unemployment for 4 months before finding a job again. Dealing with a national outbreak of pertussis in 2011-2012. And now of course COVID-19!”
Are there any current issues and trends in this field that we should be aware of?
“Good question! For vaccine preventable bacteria, COVID-19 has had a massive impact resulting in the reduction of cases of pertussis, invasive pneumococcal disease and H. influenzae, but these are starting to pick up again. We are optimistic that the benefit of ‘real-time’ sequencing and epidemiology demonstrated for SARS-CoV-2 can be translated to other organisms.
Vaccine coverage for all vaccine-preventable diseases is important to achieve and maintain good levels. Good communication in public health messages is key.
I would also include the interactions and greater integration of public health microbiology and epidemiology with other disciplines including bioinformatics, immunology, human genetics and modelling.
For us Public Health England is to be replaced by the UK Health Security Agency (for UK-wide public health protection and infectious disease capability), so we have yet to see what this means to us locally.”
What has been your most successful post and why has it made you successful?
“I would say my current one as Laboratory Surveillance Lead for Vaccine Preventable Bacteria. I believe the greater interaction with colleagues in the Immunisation and Countermeasures Division has helped the team to an improved appreciation of the impact of their work. I also recognise that I am very fortunate to have a great team with many complementary skills and although I carry overall accountability for my work area, I operate with considerable freedom.”
Do you feel like you’re making a difference in your job?
“Yes!”
What skills are the most crucial to succeeding in this career? What type of person do you need to be?
“That’s a difficult one to answer. Qualifications can obviously help, but for laboratory work you have to have good technical skills and now also IT, numerical and analytical skills. Other qualities that would help are: patience, attention to detail, decisiveness, independence and teamworking. Also problem-solving, comprehension of work-related documents, instructing and training others. I would say you need to be flexible and should seek and take any opportunities you can. Finally, as you progress you will need to develop leadership and management skills.”
How does your position fit in within the Biomedical science field?
“Healthcare science encompasses two of the main roles I am familiar with, Biomedical Scientists and Clinical Scientists, both of which are protected names and require registration with the Health and Care Professions Council (https://www.hcpc-uk.org/) @The_HCPC. In my current role as a Consultant Clinical Scientist, I lead a team of Biomedical Scientists, Clinical Scientists and Healthcare Scientists.”
Do you have any advice or tips you would give to the future generation interested in working in a laboratory setting?
“Definitely find out as much as you can about the positions you are interested in before you apply. When you see ‘contact X for an informal chat/to find out more about the post’ on an advert, do it!”
If you could do it all over again, would you choose the same for yourself? If not, what would you change?
“Yes.”
And finally, What does being a healthcare scientist mean to you?
“Being a professional, responding to public health needs and leading my team to provide an excellent service.”
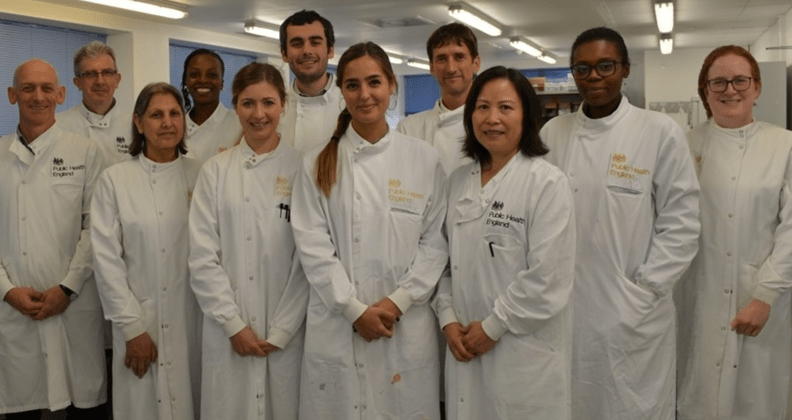
Left to right: David Litt, Norman Fry, Ginder Mann, Seyi Eletu, Alice Enefer, Samuel Rose, Alba Redin*, John Duncan, Fu Li, Karina Micah, Carmen Sheppard.
(Not in picture: Thinushaa Uthayakumaran, Malika Koulmi, Dania Vicente, René Munro; *Now at Hospital Sant Joan de Déu, Barcelona)

A special thanks to Norman Fry for allowing me to interview him. I hope this post showed everyone what an amazing job the Biomedical Scientist’s team does for Public Health England and how they keep us all safe. I hope this post has given those who didn’t know what a reference Microbiology laboratory is, a chance to see what happens behind the scenes.
Give Norman a follow on Twitter: @NormFry2013 to see how his work continues
Thank you for taking your time in reading this post, please leave a comment and subscribe.
Leave a comment