Welcome back to another Immunology case study. This case study is on Coeliac Disease.
So, sit back, grab a cuppa and happy reading!
What is Coeliac?
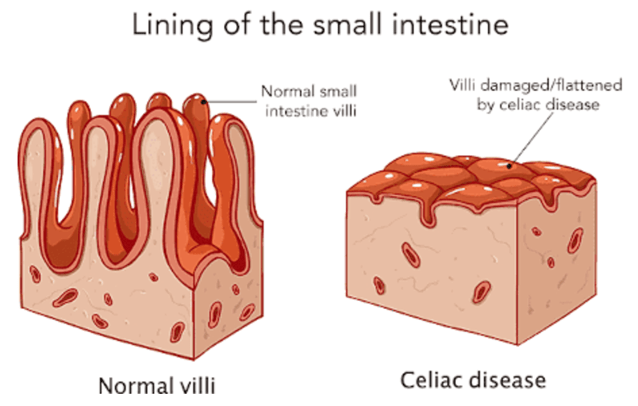
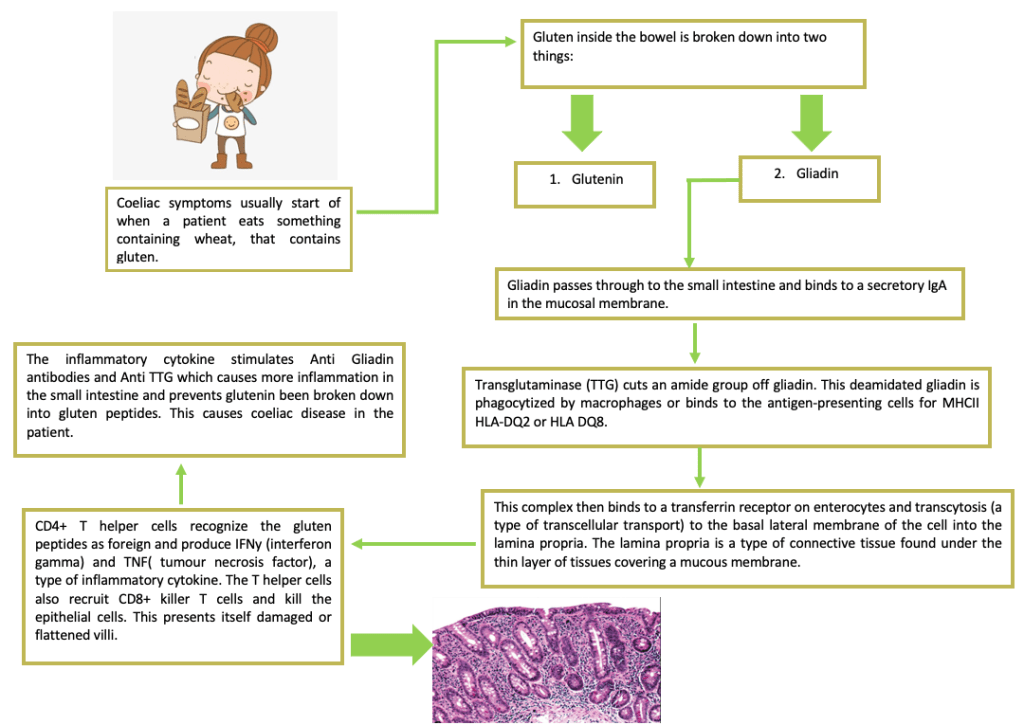
Coeliac disease is an autoimmune disease of the intestine caused by the consumption of gluten. The immune system reacts to gluten, gliadin and glutenin proteins found in wheat. This results in a Type IV hypersensitivity (cell mediated) response. When the disease manifests within the body it appears as an atrophy of the small intestinal villi and gives it a classic ‘flat mucosa’. This results in the patient having the inability to absorb nutrients leading to mal absorption.
Pathophysiology of Coeliac:
Symptoms:
Symptoms in adults:
- Chronic Diarrhea
- Bloating
- Constipation
- Indigestion
Symptoms in children:
- Abdominal pain
- Failure to thrive
- Diarrhea
Coeliac epidemiology:
Coeliac disease is a common disease in Europe and USA which affects all age groups. It is twice as common in females as in males and is seen in 5-15% of family members. This rises to 70% in identical twins. The disease can manifest at any age, with a peak on set in early childhood.
Coeliac disease is also HLA associated and it has been associated with carriers of HLA-DQ2 and HLA-DQ8. These two genes are used as gene markers to determine if a child is at high risk of developing coeliac disease.
Case Study:
A 5-year-old patient was showing symptoms of coeliac disease. Indirect immunofluorescence on endomysial antibody showed to be positive and TTG IgA results; >250.0 u/ml, was higher than the given reference range of <15.0. This was the first test the patient had for the diagnosis of Coeliac disease and following the ESPGHAN guidelines, a second positive result can be used to diagnose the patient with a coeliac disease without the need for endoscopy.
A patient result can also determine whether they have a gluten-free diet. If a patient is having a gluten-free diet their antibody titer levels will be down and if a patient is having a gluten diet results will show an increase in antibody levels. A gluten-free diet is recommended for patients with Coeliac disease to control antibody levels. This also provides clinicians with information on how well a patient is controlling their diet.
Testing for Coeliac disease:
We test for coeliac disease by testing for Tissue Transglutaminase (TTG) antibodies on our Bioplex which is a multiplex bead assay. We measure TTG levels based on the TTG complex detected using a laser built into the analyzer which gives a concentration level of the TTG complex present. Another test we carry out includes the use of indirect immunofluorescence staining of anti-endomysial antibodies on the monkey esophagus. Finally, the gold standard test for diagnosing the coeliac disease is the intestinal biopsy to identify damage to villi
What are the ESPGHAN guidelines?
The ESPGHAN guideline was introduced as a “no biopsy” for Coeliac disease diagnosis. This mainly arose from how the disease is commonly diagnosed in children. The No biopsy approach in accordance with the guideline has been shown to be safe in children that show high TTG-IgA 10 times the upper limit of normal with an appropriate and positive endomysial antibody in a second serum sample. An example of this can be seen in the case study above. A biopsy is carried out on a child if it is a positive TTG-IgA result but with lower titers. Patients should have ≥4 biopsies from the distal duodenum and ≥1 from the bulb, during a gluten-containing diet.
Is the ESPGHAN guideline beneficial for the patient?
The ESPGHAN guideline is a good guideline to stop patient’s from getting a biopsy. Coeliac disease; in most cases is diagnosed at a young age, this guideline is beneficial for young patients as it saves them from having a biopsy done. It also provides a faster diagnosis for the patient so they can start a strict non-gluten-free diet. By the ESPGHAN guideline, HLA testing is not required if a patient has tested positive for TTG-IgA. However, if a parent had coeliac disease, their children should have HLA testing carried out to see if they are carriers of HLA-DQ2 and HLA-DQ8 genes. This will be if they are at high risk of developing coeliac disease. This provides the parent with information on the symptoms to look out for and a more controlled diet, as well as an early diagnosis.
Thank you to everyone for reading. I hope you found this informative and it gave you a little insight of one of the many conditions we diagnose in Immunology.
Leave a comment