It has been a long time since I have written a case study and posted on my blog page. Life got in the way and I guess I took a step back to just enjoy and breathe.
But here is a case study, so, sit back grab a cuppa and HAPPY reading!!
Pollen Food Allergy Syndrome
Within our 7.88 billion human population, they are a group of people who tend to develop allergies to substances they have exposure to, especially pollen. For this group, something as simple as eating an apple in the park could prove fatal.
It may sound strange, but it is true.
These people have a condition known as Pollen Food Allergy Syndrome (PFAS).
PFAS Pathophysiology:
When a person has a pollen allergy, their immune system develops specific allergic antibodies.
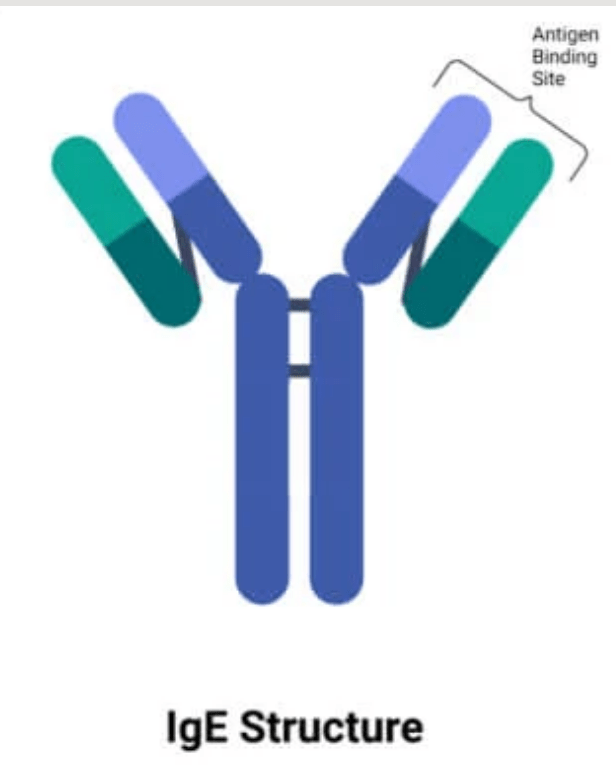
People are now aware of what antibodies are after our recent pandemic. However, antibodies are a lot more complicated.
Did you know there are five different antibodies? Each of these five antibodies has a specific role in our immune system.
As this case study is focusing on allergy, we will be focusing on IgE antibody. IgE antibodies are created against the substances you are allergic to. In this case, IgE antibodies towards pollen.
Having an allergy to pollen is known as Allergic Rhinitis, a fancier term for Hay Fever.
Those people that have hay fever and decide to eat fresh or raw fruits and vegetables can end up with itching or even swelling of their mouth and tongue.
Now, I bet you’re wondering how does having hay-fever be linked to developing the itchy in your mouth??
Well, this is due to something called cross reactivity.
Cross Reactivity
Specific-IgE (S-IgE) to common pollen that are circulating around the body cross-react between allergens found in pollen within fruit and vegetables after contact with the oral cavity (the mouth). The reason for cross reaction is due to the plant derived allergen been similar to a common pollen the person might be allergic to.
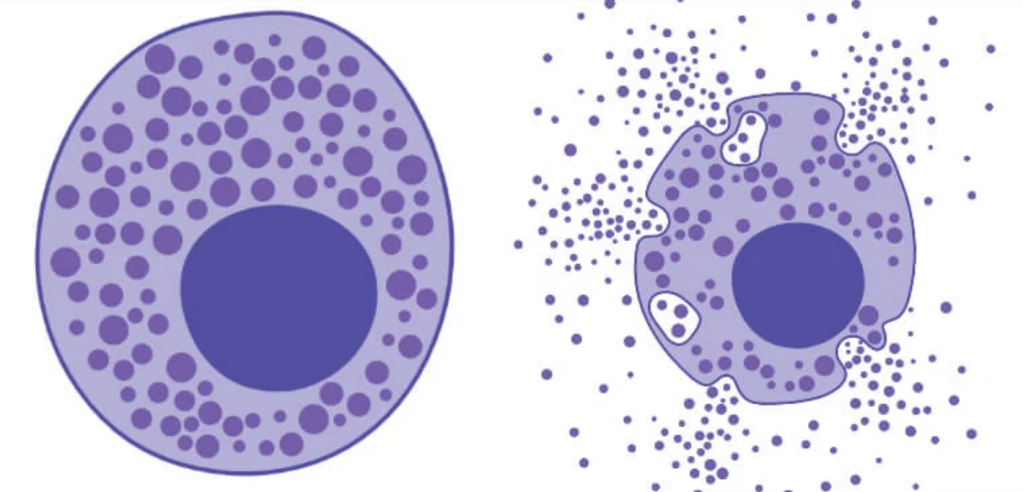
The cross reactivity and bonding of the fruit/ vegetable allergen to a specific IgE to a common pollen results in mast cell degranulation resulting in physical symptoms.
This case study is going to focus on the population that develop allergies towards pollen and it’s link to the itchy sensation after eating a certain fruit or vegetable.

Epidemiology:
PFAS is the most widespread food allergy that affects millions of people with respiratory allergies.
The type of PFAS depends on a variety of factors. These factors include the type of sensitization and the cross-reactivity patterns of these allergens. The different factors also vary in geographical regions. For example, In central and northern Europe, individuals tend to be sensitized to birch, grasses, and mugwort pollens. But in the Mediterranean areas, individuals are more likely to be sensitized to grasses and ragweed pollens.
The prevalence of PFAS is increasing and it is increasing with the incidence of respiratory allergies.
How is PFAS tested for in the laboratory:
We test for PFAS using the Phadia 250 ImmunoCap. The Phadia 250 immunoCAP allows the formed specific IgE antibody in the patient’s serum sample towards the allergen to bind to the antigen on the immunoCAP. This creates an antigen and antibody complex. The concentration of the antigen and antibody complex present in the patient’s serum is read by a fluorometer. The higher the antigen and antibody complex concentration level, the more exposure the patient has had to allergen.
The ImmunoCAP also carries out allergen component testing. Testing with allergen components measures allergic sensitization to molecules found within whole allergens.
Component testing allows a deeper understanding of causes, risks, and management of symptoms. It does this by knowing which protein a patient may be reacting to, which allows a greater understanding of their potential allergy. Component testing is useful when testing for cross-reactivity within patients.

Case study:
A 13 year old patient was complaining of having an itchy mouth and swollen lips after a day of eating peaches, strawberries and oranges on a picnic. The patient visited an allergy clinic and blood was taken and then run on our Phadia 250.
Patient results:
| Total IgE | 112 KU/L |
| Orange | <0.35 Kua/ L |
| Silver Birch | 8.71 Kua/ L |
| Strawberry | <0.35 Kua/ L |
| Pineapple | <0.35 Kua/ L |
| rPru p1, LTP, (Peach component) | 2.87 Kua/ L |
| rPru p3, LTP, (Peach component) | 1.49 Kua/L |
| rPru p4, prof, (Peach component) | <0.35 Kua/ L |
| Betv 1 (Birch pollen component) | 8.73 Kua/L |
Reference range:
| Grade 0 | Negative | <0.35 Kua/ L |
| Grade 1 | Weak positive | 0.35- 0.69 Kua/L |
| Grade 2 | Positive | 0.7- 3.5 Kua/L |
| Grade 3 | Positive | 3.5-17.5 Kua/L |
| Grade 4 | Positive | >17.5 Kua/ L |
The patient shows high levels of specific IgE towards silver birch, specifically the Betv1 Birch component and peach components.
The results suggest that the patient has IgE towards silver birch, particularly Betv 1. The results also show IgE towards rPru p1 and rPru p3 (a major peach allergen).
Going back to cross-reactivity, it is known for rPru p3 to cross-react with silver birch. In this case, we can see that the patient has PFAS due to his allergy to silver birch cross-reacting with rPru p3, due to being similar, resulting in the patient developing an itchy mouth and tongue.

What happens next to our peach loving patient?
The patient will get a referral to the allergy clinic where they will be given advice on how to handle their allergies. This could include not eating anything with peaches and using cetirizine or steroid nasal spray for pollen season. Depending on the severity of the reaction they will also be asked to carry an Epipen.

Common pollen related reactions
| Celery | Mugwort | Birch |
| Celery | Mugwort | Spice |
| Mugwort | Mustard | |
| Mugwort | Peach | |
| Ragweed | Melon | Banana |
| Plantain | Melon | |
| Pellitory | pistachio |
Did you know that a person can also develop pollen unrelated reactions, here are some examples:
| Latex | Fruits |
| Mites | Snails |
| Bird | Eggs |
I have given the spotlight to the hay-fever folks, but now it’s time for non allergic individuals to shine.
A non-allergic individual can develop food contact hypersensitivity syndrome. It usually presents itself as a hive. Hypersensitivity syndrome occurs due to foods such as pineapple or red wine containing histamine or other vasoactive amines (serotonin or tyramine). Another cause could also be the food for example strawberries or tomatoes causing direct histamine release from mast cells without the presence of IgE.
Physical Symptoms:
- Tingling
- Pruritus (itching of skin)
- Erythema (Red, raised, blotchy skin)
- Angioedema (swelling) of lips, tongue and soft palate
I hope everyone enjoyed reading this posts on Pollen Food Allergy Syndrome and found it informative on what it is and how we test for it in our immunology laboratory.
Leave a comment on your thoughts on this post.
Thank you!!
Leave a comment